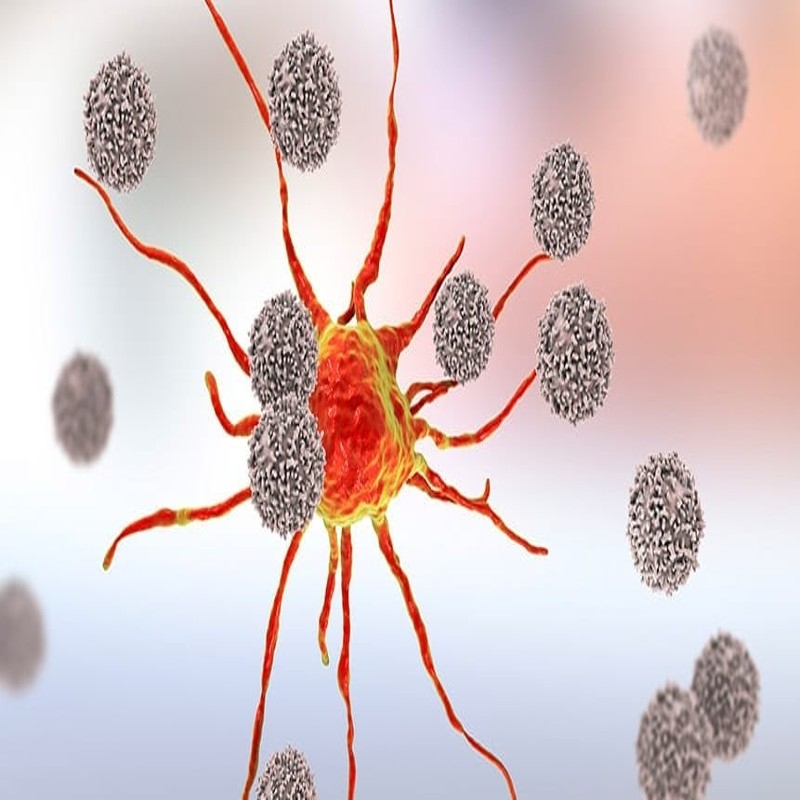
Immunotherapies have revolutionized the treatment landscape for metastatic melanoma over the past decade. Checkpoint inhibitors like ipilimumab, nivolumab, and pembrolizumab work by removing the brakes on the immune system allowing T cells to recognize and attack cancer cells. Ipilimumab was the first FDA-approved immunotherapy for metastatic melanoma in 2011. It works by targeting CTLA-4, a protein receptor that downregulates the immune system. In phase 3 trials, ipilimumab doubled median overall survival compared to gp100 vaccine alone. Nivolumab and pembrolizumab are PD-1 inhibitors that target another immune checkpoint, PD-1. Both drugs showed superior response rates and progression-free survival compared to chemotherapy or ipilimumab in phase 3 trials leading to their FDA approval in 2014. Response rates to PD-1 inhibitors are around 40-45% and some patients experience long term remissions. Combination immunotherapy using ipilimumab plus nivolumab resulted in longer progression free and overall survival than ipilimumab alone in a phase 3 study, leading to FDA approval of this combination in 2015.
Targeted Therapies
For Metastatic Melanoma Therapeutics patients whose tumors harbor BRAF mutations, targeted therapies that inhibit BRAF or combine BRAF and MEK inhibitors have become standard of care. About 50% of melanomas have an activating BRAF V600E or V600K mutation. Vemurafenib was the first FDA-approved BRAF inhibitor in 2011 and demonstrated superior response rates and progression free survival compared to dacarbazine in phase 3 trials. Dabrafenib is another BRAF inhibitor approved in 2013 based on improved response and progression free survival over dacarbazine. While initially effective, most patients develop resistance within a year of BRAF inhibitor monotherapy due to reactivation of the MAPK pathway. Dabrafenib plus trametinib, a MEK inhibitor, became the new standard of care based on improved progression free and overall survival compared to vemurafenib or dabrafenib monotherapy in phase 3 studies leading to approvals in 2014. For patients who progress on BRAF inhibitors, other targeted therapies continue to be investigated.
Combination Therapies
Given the complementary mechanisms of action of immunotherapies and targeted therapies, combining the two approaches holds promise. In a phase 1 trial, the addition of the PD-L1 inhibitor atezolizumab to vemurafenib and cobimetinib improved response rates and progression free survival over vemurafenib and cobimetinib alone. Phase 3 studies are ongoing to validate this combination. There is also interest in combining immunotherapy earlier in the treatment sequence, before or concurrently with targeted therapy. For example, a phase 3 trial is testing nivolumab plus low dose ipilimumab before and after BRAF/MEK inhibitor therapy. Additional studies are exploring using immunotherapy after progression on targeted therapy to potentially overcome acquired resistance. The goal is to leverage synergy between stimulating the immune system alongside inhibiting oncogenic drivers to maximize clinical benefit for metastatic melanoma patients.
Clinical Challenges
While immunotherapies and targeted therapies have transformed metastatic melanoma treatment, many challenges remain. Only a subset of patients experience long term remission or cure with current therapies. Better predictive biomarkers are needed to select patients most likely to respond to a specific treatment approach. Understanding acquired resistance mechanisms will aid development of newer agents to overcome resistance. Managing immune related adverse events from checkpoint inhibitors also requires expertise. Finally, only a fraction of melanomas harbor BRAF mutations, so novel targeted approaches are still needed for BRAF wild type disease which has proven more difficult to treat. Further research to address these challenges will continue advancing care for patients with metastatic melanoma.
Get more insights on Metastatic Melanoma Therapeutics
Recent Advances in Treating Metastatic Melanoma Therapeutics