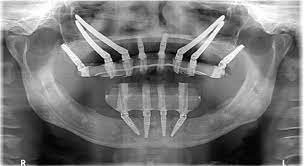
Zygomatic Implants in Dubai, a specialized field within dental implantology, presents its own set of challenges that practitioners must navigate for successful outcomes. Zygomatic implants are long, angled implants used when traditional implant placement is not feasible due to bone loss in the maxillary region. Despite their efficacy, various issues can arise during the zygomatic implant procedure. Here, we explore common challenges and their corresponding solutions in zygomatic implantology.
One prevalent challenge is the anatomical complexity of the maxillary sinus and the zygomatic bone. The proximity of vital structures such as the maxillary sinus and the orbit poses a risk during implant placement. To address this, thorough preoperative assessment, including advanced imaging techniques like cone-beam computed tomography (CBCT), is essential. Additionally, using computer-guided implant placement can enhance precision and minimize the risk of damaging adjacent structures.
Another common issue is the limited availability of bone in the posterior maxilla. When severe bone resorption occurs, traditional implant placement becomes challenging. Zygomatic implants, which engage the dense zygomatic bone, offer a solution. However, achieving optimal stability in this compromised bone environment remains a concern. Augmentation techniques, such as sinus floor elevation or bone grafting, may be employed in conjunction with zygomatic implants to enhance stability and ensure long-term success.
Complications related to prosthesis design and fabrication can also arise. Achieving proper occlusion and functional harmony is crucial for the longevity of zygomatic implants. Dentists must carefully consider the design of the prosthesis and verify its accuracy through meticulous clinical and laboratory procedures. Occlusal adjustments and regular follow-ups are necessary to prevent complications such as implant overloading and peri-implantitis.
Infection control is a universal concern in implantology, and zygomatic implant procedures are no exception. The close proximity of the zygomatic implants to the sinus and nasal cavities increases the risk of postoperative infections. Strict adherence to aseptic techniques during surgery, prophylactic antibiotics, and patient education on postoperative care are essential measures to minimize the risk of infections.
Patient management plays a pivotal role in addressing challenges in zygomatic implantology. Patients with severe maxillary atrophy often present with compromised general health. Managing their expectations, ensuring their overall health is optimized, and addressing systemic issues are crucial steps in achieving successful outcomes. Collaboration with other healthcare professionals may be necessary to address systemic conditions that could impact the implant procedure.
Postoperative complications, such as implant failure or peri-implantitis, can occur despite meticulous planning and execution. Regular follow-ups, patient education on oral hygiene, and early intervention in case of any signs of complications are crucial. Additionally, continuous professional development for the dental team is essential to stay updated on the latest advancements and techniques in zygomatic implantology.
In conclusion, while zygomatic implantology provides a viable solution for patients with severe maxillary atrophy, it comes with its own set of challenges. The key to overcoming these challenges lies in meticulous planning, advanced imaging, precise surgical techniques, and comprehensive patient management. By addressing anatomical complexities, bone deficiencies, prosthesis-related issues, infection control, and postoperative complications, practitioners can enhance the success rates and longevity of zygomatic implant procedures, ultimately improving the quality of life for patients with complex maxillary conditions